Dr. Gary S. Goldberg from Rowan University details a study he co-authored that was published by Oncotarget in 2015 and entitled, “Antibody and lectin target podoplanin to inhibit oral squamous carcinoma cell migration and viability by distinct mechanisms.”

Behind the Study is a series of transcribed videos from researchers elaborating on their oncology-focused studies published by Oncotarget. A new Behind the Study is released each Monday. Visit the Oncotarget YouTube channel for more insights from outstanding authors.
—
Speaker
Welcome to the Oncotarget YouTube channel. This interview is with Dr. Gary Goldberg in the departments of Molecular Biology, Cell Biology and Pathology at the School of Osteopathic Medicine, Rowan University, Stratford, New Jersey. They’re talking about their manuscripts published in Volume 6, Issue 11 of Oncotarget titled, “Antibody and lectin target podoplanin to inhibit oral squamous carcinoma cell migration and viability by distinct mechanisms.“
Dr. Gary Goldberg
Okay, so the name of the paper that we published is, “Antibody and lectin target podoplanin to inhibit oral squamous carcinoma cell migration and viability by distinct mechanisms.” What brought us around to this work was actually looking at how tumor cells behave in their microenvironment, and that’s critically important because the cancer originally was a normal cell. It became a cancer cell, and it’s actually controlled by the normal cells that surround it, and it needs to escape this control to become malignant and metastatic. The vast majority, over 90%, of deaths are actually due to metastasis.
So what we did is we looked at all of the different genes and proteins that are regulated to overcome this process of contact normalization. In other words, they overcome the ability of the normal cells to control them so they can invade and multiply and basically realize their malignant potential. And when we did this, we basically looked at over 30,000 different genes and we found this one receptor really rose to the top of all of them, and this receptor is called podoplanin, or PDPN is the symbol. What this does is it basically enables tumor cells to migrate, to escape from their microenvironment and metastasize into new areas and basically become very, very aggressive cancers.

Now, how do we target the podoplanin? Well, there were antibodies developed to podoplanin, and antibody of course, is a great therapy. We understand that there were many potential uses for antibodies, but normally these are very drastic approaches where a patient is either injecting themselves or going into a clinic where they have infusions of antibodies and they can not be eaten, in other words. So they’re not very useful for preventative treatments when someone does not yet have the disease. Cancer, of course, is something we want to catch very early. The earlier we catch it, the better the results will be. We pretty much know this.
And so, we identified a compound, which we call MASL, and what MASL does is it binds to the podoplanin receptor, and in very low nanomolar levels or concentrations, this inhibits the ability of the tumor cell to migrate. So right away, we’re inhibiting the malignant potential of the tumor. At higher concentrations, but pretty much still either micromolar or even sub-micromolar, we’re actually able to kill the tumor cells. And that’s some of the results that we published in this paper, is how we’re killing the tumor cells. We do not rely on apoptosis. This is a caspase-independent on non-apoptotic necrosis, and so we’re able to kill tumor cells regardless of their potential to survive other treatments, and that’s very important.
We focused on oral cancer. Standard chemotherapy drugs do not work well on oral cancer. The oral squamous cell carcinoma cells, which we studied in this paper, are very resistant to these drugs because they tend to avoid apoptosis for one reason or another. So this MASL has a great potential. The other thing about MASL is it’s orally administered. So of course, for oral cancer, the lesion is in a patient’s mouth, oftentimes this is a pre-malignant lesion, and it will not usually become cancerous until it expresses the podoplanin receptor. So by incorporating this MASL into a lozenge, for example, we hope, and we believe, that we can inhibit – or at least delay – the onset of these precancerous lesions from becoming actual cancer and they cause tremendous harm.

In the United States, for example, one person dies of oral cancer every hour, and worldwide, of course, that number is huge. We’re talking about one every 5 minutes. So there’s a huge need to treat oral cancer, and it would be much better to treat it earlier, before it actually becomes oral cancer, than later. So what we found is that these precancerous lesions, these cells that are bound to become cancer but are not yet cancer, they express this podoplanin receptor and our drug can target this receptor very quickly. As a matter of fact, what we show in the paper and what’s on the cover of that issue of the journal which has that paper in it, the MASL binds within 2 minutes. So it’s very quick and we were very surprised to see how quickly the MASL can bind to this podoplanin receptor to prevent the tumor cell migration and growth and proliferation.
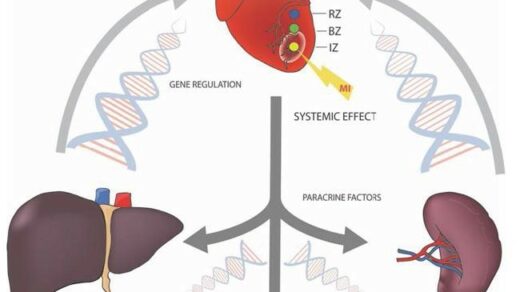
In addition to the cancer cells themselves, we also found that the cancer cells are able to induce podoplanin expression of the same receptor in the fibroblasts that surround them. So, instead of the normal cells that surrounding the tumor acting as a normalization factor to control the tumor growth, they now become cancer-associated fiberglass. And these, instead of inhibiting tumor growth, they actually promote tumor growth. They can actually destroy the extracellular matrix and allow the tumor cells to form in base of fronts in this very disrupted extracellular matrix, which would normally be very ordered. It becomes disordered.
At present, we’re in the process of initiating clinical trials to actually see how this drug might work in people, and of course, this is a very long and very complicated process in a lot of different ways, but this is the way that we’re attempting to do it.
So, basically, we have a target, that’s podoplanin, the drug in this case is MASL, and what we did is we compared it to antibodies, and we found that the dynamics are very similar and the concentrations are very similar, but of course, MASL, has the advantage of being orally administered, whereas antibodies have to be injected because they will not survive digestion, and in oral cancer, is an unmet need. So we have a disease to treat and the oral administration of the drug seems very suitable, because we would be exposing these lesions, both topically and systemically, with this process.
Click here to read the full study published by Oncotarget.
YOU MAY ALSO LIKE: More Oncotarget Videos on LabTube
—
Oncotarget is a unique platform designed to house scientific studies in a journal format that is available for anyone to read—without a paywall making access more difficult. This means information that has the potential to benefit our societies from the inside out can be shared with friends, neighbors, colleagues, and other researchers, far and wide.
For media inquiries, please contact media@impactjournals.com.