In this top-performing paper, researchers compare the overall survival, average total healthcare costs, and resource utilization among patients with advanced cancers who received standard care versus precision, targeted oncology.
The Top-Performer series highlights research literature published in Oncotarget that has generated a high Altmetric score. Altmetric scores, located at the top-left of trending Oncotarget papers, provide an at-a-glance indication of the volume and type of online attention the research has received. Read Oncotarget’s Top 100 Altmetric papers.
—
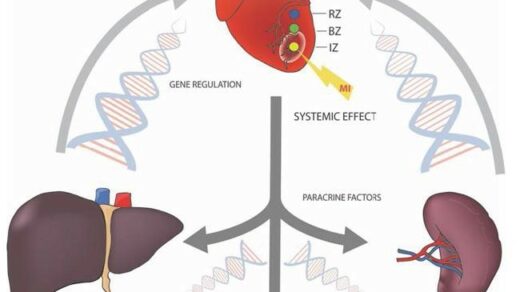
In addition to the steep emotional and physical burden of being diagnosed with an advanced cancer, most cancer patients must undergo a number of expensive procedures and treatments, which may or not improve their overall survival. Precision medicine is the personalization of healthcare by using new technologies and analyzing patient family history and individual patient characteristics to improve patient outcomes. Precision oncology is personalized cancer care.
“The use of advanced molecular diagnostic technologies, such as Next-Generation Sequencing (NGS) based gene panel testing, to select targeted therapies in advanced cancer patients is known as precision oncology [1].”
Researchers, from Intermountain Healthcare facilities (located in Utah and California, U.S.) and California’s Stanford University School of Medicine, conducted a well-read study published in 2018, titled: “Precision oncology in advanced cancer patients improves overall survival with lower weekly healthcare costs.” This paper currently presents with an Altmetric attention score of 484.
“The impact of precision oncology on guiding treatment decisions of late-stage cancer patients was previously studied in a retrospective analysis. However, the overall survival and costs were not previously evaluated.”
The Study
The researchers previously conducted a retrospective, matched control study of 72 patients with diverse subtypes of metastatic cancer and evaluated their progression free survival (PFS) and healthcare costs. Their results showed that the patients who received precision cancer medicine did not have higher costs and had longer PFS than the control group (22.9 weeks vs. 12.0 weeks). To expand on this study, the researchers evaluated a subset of 44 patients who received care from the Intermountain Healthcare system. Half of the patients received precision oncology care and half received standard therapy or best supportive care. They measured overall survival, average total healthcare costs, and resource utilization.
“Building on a matched cohort study of 44 patients with metastatic cancer who received all of their care within a single institution, we evaluated the overall survival and healthcare costs for each patient.”
Results & Conclusion
“We report the overall survival and healthcare costs associated with precision oncology in these patients with advanced cancer.”
The researchers found in their results, through extensive comparative data, an overall survival benefit for patients who receive targeted therapy based on genomic testing when compared to the cohort of patients who received standard therapy or best supportive care. They also found that resources used and associated with health services were 40% lower in the precision oncology group across all sites of care.
The average weekly costs of care for patients receiving precision oncology were also lower than for those in the control group, however, researchers explain that patients in the precision oncology group have higher upfront prescription drug costs and sequencing charges. In addition, the overall cost of their care is extended over a significantly longer period of time, given their longer overall survival achieved through precision medicine.
“The simultaneous improvement in overall survival, as well as lower per-week costs, suggest that a precision medicine approach may be an attractive option for refractory cancer patients. Lower inpatient costs during the last three months of life appears to be a major source of the cost savings observed in the targeted treatment group.”
“These findings suggest that precision oncology may improve overall survival for refractory cancer patients while lowering average per-week healthcare costs, resource utilization and end-of-life costs.”
Click here to read the full scientific study, published in Oncotarget.
—
Oncotarget is a unique platform designed to house scientific studies in a journal format that is available for anyone to read—without a paywall making access more difficult. This means information that has the potential to benefit our societies from the inside out can be shared with friends, neighbors, colleagues and other researchers, far and wide.
For media inquiries, please contact media@impactjournals.com.