Researchers perform a phase three subgroup analysis study demonstrating positive results in patients with HPV-negative oropharyngeal cancers due to the addition of weekly nimotuzumab doses while receiving cisplatin and radiation treatment.
The Trending with Impact series highlights Oncotarget publications attracting higher visibility among readers around the world online, in the news, and on social media—beyond normal readership levels. Look for future science news and articles about the latest trending publications here, and at Oncotarget.com.
—
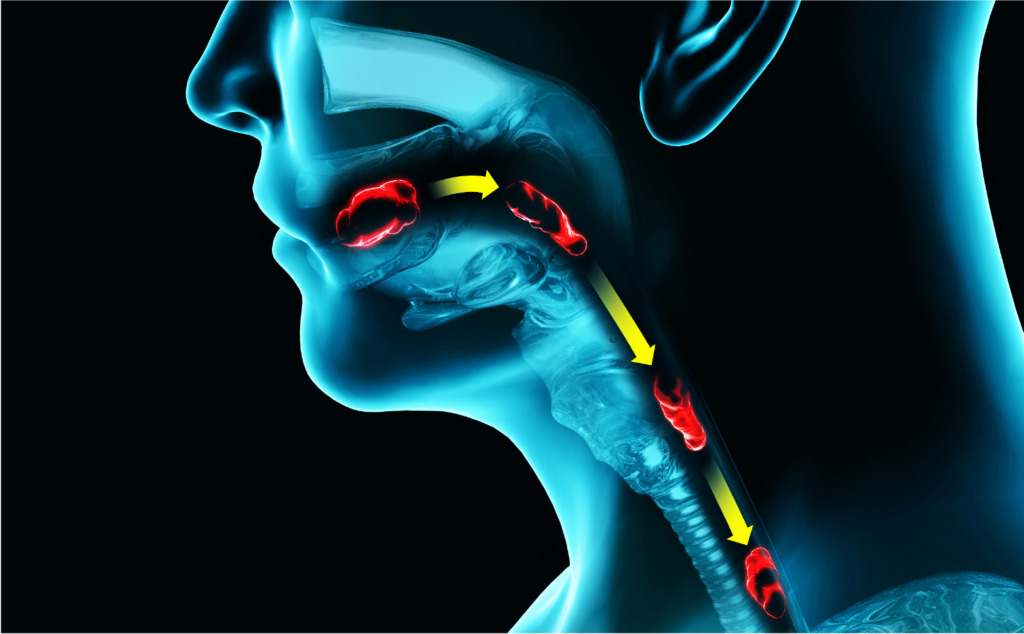
Each year, oral cancer accounts for around 53,000 new patient diagnoses in the United States. However, the highest number of cases of oral cancer in the world are found in India (primarily due to tobacco use)—and researchers say this number is increasing. Oral cancer in any part of the oropharynx (the back-third of the tongue, tonsils, soft palate, and back and sides of the throat) is called oropharyngeal cancer.
“As opposed to HPV related oropharyngeal cancer, HPV negative oropharyngeal cancers have worse prognosis.”
Researchers from Tata Memorial Hospital and Tata Memorial Centre in Mumbai, India, previously reported that in a phase three randomized study of an epidermal growth factor receptor inhibitor and targeted chemotherapy, called cetuximab, they showed a trend towards improvement when used in patients with locally advanced head and neck cancers. Compared with results in other similar studies, they believe their results were likely due to a younger cohort of patients with predominantly HPV-negative diseases.
“Taking this into consideration, we decided to perform a subgroup analysis of the HPV negative oropharyngeal cancer cohort, to study the absolute improvement in 2-year outcomes with the addition of nimotuzumab. We compared 2 year progression free survival (PFS), disease free survival (DFS), locoregional control (LRC) and overall survival (OS) between both arms.”
The Study
“HPV negative oropharyngeal cancer has unsatisfactory treatment outcomes and is a candidate for escalation of treatment. We wanted to determine whether the addition of nimotuzumab to cisplatin-radiation could improve outcomes in these poor-risk tumors.”
In this study, the researchers analyzed 536 patients undergoing definitive chemoradiation for locally advanced head and neck cancers, with 269 having a primary tumor located in the oropharynx. Of these patients, 187 were p16 protein (HPV) negative and divided into two treatment arms: 91 participants in the cisplatin-radiotherapy (CRT) treatment arm and 97 in the nimotuzumab-cisplatin-radiotherapy (NCRT) treatment arm. Nimotuzumab is an antibody drug and radiosensitizer that binds to the epidermal growth factor receptor.
The participants consisted of a total of 21 females, therefore the cohort was primarily male, of median age 54.5, reported tobacco use in 90%, and 80% were in disease stage IV. Patients in the CRT treatment arm were given 30mg/m2 of cisplatin weekly, in addition to radiation therapy. In the NCRT treatment arm, in addition to radiation therapy and 30 mg/m2 of cisplatin, patients received 200 mg of nimotuzumab weekly.
Results
In the larger cohort, researchers found that the HPV positive/negative interaction test using immunohistochemistry staining taken by each participant was a significant determinant in progression free survival, locoregional control, and overall survival, but not in disease free survival. In the sub-group analysis, their data shows that the addition of nimotuzumab has a differential patient impact on disease free survival with respect to HPV status.
In the NCRT sub-group, improvement in locoregional control by nimotuzumab was largely responsible for patient improvement in progression free survival. On average, time to locoregional failure in the CRT treatment arm was 17.3 months, and in the NCRT treatment arm, it was 60.3 months. The team also found that the addition of nimotuzumab led to an 18.6% improvement in 2-year overall survival, jumping from 39.0% to 57.6%.
“Locoregional control, progression-free survival and overall survival were improved with the addition of nimotuzumab to cisplatin and radiation.”
Conclusion
“The addition of nimotuzumab to weekly cisplatin-radiation improves outcomes inclusive of overall survival in HPV negative oropharyngeal cancers.”
“The results of the current study clarify the importance of treatment intensification in HPV negative oropharyngeal cancers.”
Click here to read the full scientific study, published in Oncotarget.
—
Oncotarget is a unique platform designed to house scientific studies in a journal format that is available for anyone to read—without a paywall making access more difficult. This means information that has the potential to benefit our societies from the inside out can be shared with friends, neighbors, colleagues and other researchers, far and wide.
For media inquiries, please contact media@impactjournals.com.